Long-term care facilities are starting to see long-awaited signs of post-pandemic life, with residents and staff largely vaccinated and loosened state restrictions now allowing for some gatherings and in-person visits from family.
Get Instant Access to This Article
Subscribe to Worcester Business Journal and get immediate access to all of our subscriber-only content and much more.
- Critical Central Massachusetts business news updated daily.
- Immediate access to all subscriber-only content on our website.
- Bi-weekly print or digital editions of our award-winning publication.
- Special bonus issues like the WBJ Book of Lists.
- Exclusive ticket prize draws for our in-person events.
Click here to purchase a paywall bypass link for this article.
From the start of the coronavirus pandemic, long-term care facilities and nursing homes were in a precarious spot, caring for many of their communities’ highest-risk residents.
They were dealt a disproportionate brunt of the pandemic, with at least 990 deaths at such facilities in Worcester County, or 45% of all deaths in the county, according to the Massachusetts Department of Public Health. Their residents were long forced into isolation and their workers at high risk of catching the virus themselves.
Now, about a year after cases reached their initial peak locally last spring, these care facilities are starting to see long-awaited signs of post-pandemic life, with residents and staff largely vaccinated and loosened state restrictions now allowing for some gatherings and in-person visits from family.
“We’ve come a long way,” said Vin Librandi, the COO of Worcester’s Jewish Healthcare Center, a facility including assisted living, hospice, long-term care and other facilities.
The Jewish Healthcare Center was among the area’s hardest hit facilities early in the pandemic. Early last April, when Worcester County’s case total was a little over 100 – it’s more than 70,000 today – the center made headlines for having three residents die from the virus. At the time, such a total at once was unusual.

Like hospitals and other health centers, long-term care facilities and nursing homes quickly went into lockdown. Visitors weren’t allowed – even sometimes in a patient’s last moments. That left an already burdened staff to act as close to family as could be.
“Our staff became their families,” Librandi said.
Turning the corner
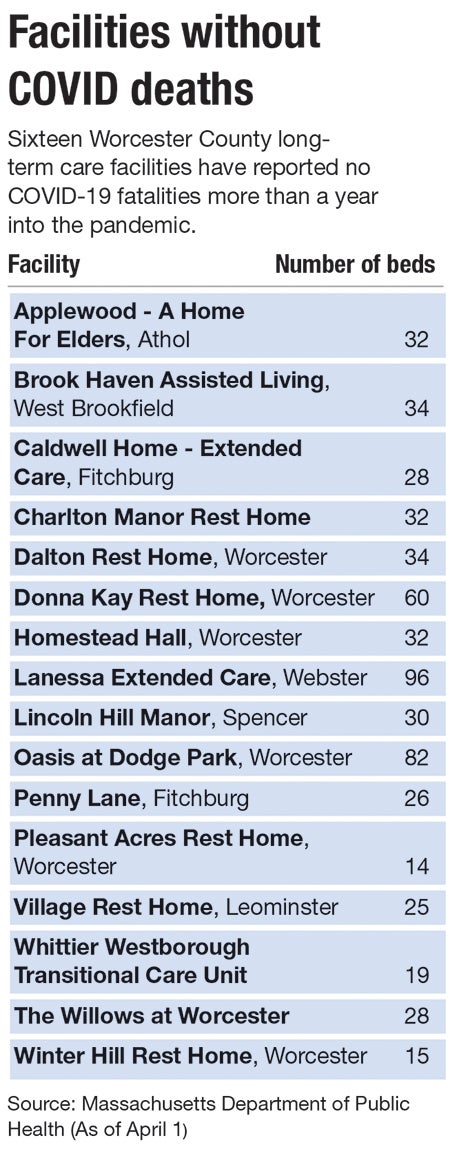
A year later, 22 long-term care facilities in Worcester County have recorded 20 or more coronavirus deaths. Facilities are still required to test their staff every other week and report results to the state, despite nearly everyone being vaccinated.
Finally, though, better days are ahead.
Most Department of Public Health restrictions are still in place, such as both patients and visitors wearing facial coverings and keeping distance for most of the visit, as well as visitors having passed a screening. But in mid-March, the state allowed for the first time since the pandemic began in earnest for visitors to make physical contact with their loved ones, at last allowing hugs once given up for the sake of social distancing.
“That’s huge,” Jackie Carey, the assistant administrator at Applewood Home for Elders in Athol, said of allowing physical embraces again.
As a sign of just how seriously state health leaders continue to take the pandemic, even those hugs retain a few more restrictions: Faces must be in opposite directions, and hand sanitizer has to be used before and after.
“We’re still very cautious,” said Brenda Turner, the manager of Lincoln Hill Manor in Spencer, a rest home and assisted living facility. “It’s working for us. We’ve been very fortunate.”
Applewood Home for Elders, a 32-bed facility that’s yet to report a coronavirus death, is staying strict, too. It allows 30-minute visits in its conference room, sanitizing between each one. With residents still unable to go out much, those visits are critical to their mental wellbeing, Carey said.
Kate Columbus, the nursing director at the Jewish Healthcare Center, agreed. Patients' mental toll was clear, she said.
“Some haven’t seen their family in a year,” Columbus said. For a time, she added, it was even more restrictive. “Not only were they isolated from their families, they were also isolated from each other.”
Vaccinations driving progress
What’s allowing for looser restrictions now is simple: Nearly all patients and staff at such facilities are vaccinated, with a small number of exceptions made for religious or health reasons. Older residents and those with certain health risks were prioritized for vaccines.
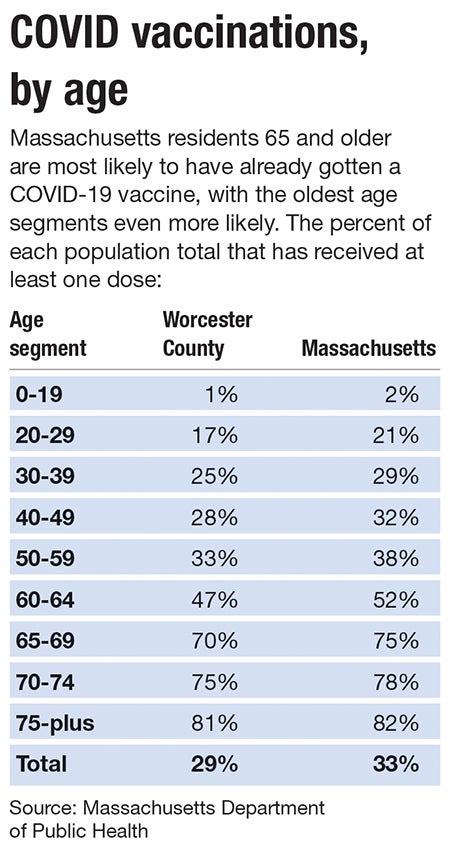
More than 332,000 state residents 75 or older are fully vaccinated, and another 305,000 who are 65 or older, according to the DPH. Another nearly 289,000 between those two age groups have received at least one dose as of April 1. Those 50 and older make up even far larger numbers.
A few numbers indicate how disproportionate those numbers are: Those 75 and older make up 7% of the Massachusetts population but 18% of those who’ve received at least one dose.
Facilities have also touted extra precautions.
Eisenberg Assisted Living, part of the Jewish Healthcare Center, upgraded its ventilation system so indoor air is only from the outdoors – nothing recirculated from elsewhere inside the building. The staff bought a carbon dioxide meter to measure common spaces to ensure enough fresh air, and an ultraviolet light to sanitize high-traffic areas.
“The difference in adding those, it was huge,” Columbus said of the new equipment. Like other local care facility leaders, her feeling these days is largely one of relief and cautious optimism.
“The resilience of some of our folks has been quite remarkable,” she said.

