The pandemic has complicated things for Behavioral health providers in their patients in two major ways: anxiety of getting the virus and depression from being stuck often alone indoors has increased risks for patients, while efforts to keep people generally away from one another has made group therapy sessions almost impractical.
Get Instant Access to This Article
Subscribe to Worcester Business Journal and get immediate access to all of our subscriber-only content and much more.
- Critical Central Massachusetts business news updated daily.
- Immediate access to all subscriber-only content on our website.
- Bi-weekly print or digital editions of our award-winning publication.
- Special bonus issues like the WBJ Book of Lists.
- Exclusive ticket prize draws for our in-person events.
Click here to purchase a paywall bypass link for this article.
Behavioral health providers were already dealing with a crisis before the coronavirus outbreak hit, with sky-high opioid use and fast-rising suicide rates.
The pandemic has complicated things for clinicians and their patients in two major ways: anxiety of getting the virus and depression from being stuck often alone indoors has increased risks for patients, while efforts to keep people generally away from one another has made group therapy sessions almost impractical.
Providers spent weeks as the pandemic began hitting hard in March scrambling to figure out how to keep inpatient areas safe and move therapy sessions from in-person to online.

“It’s remarkable the level of anxiety people are under,” said Catherine Collins, the regional business development liaison at Spectrum Health Systems in Worcester, who has been in addiction recovery for more than 20 years. “It’s exactly what could lead people to relapse.”
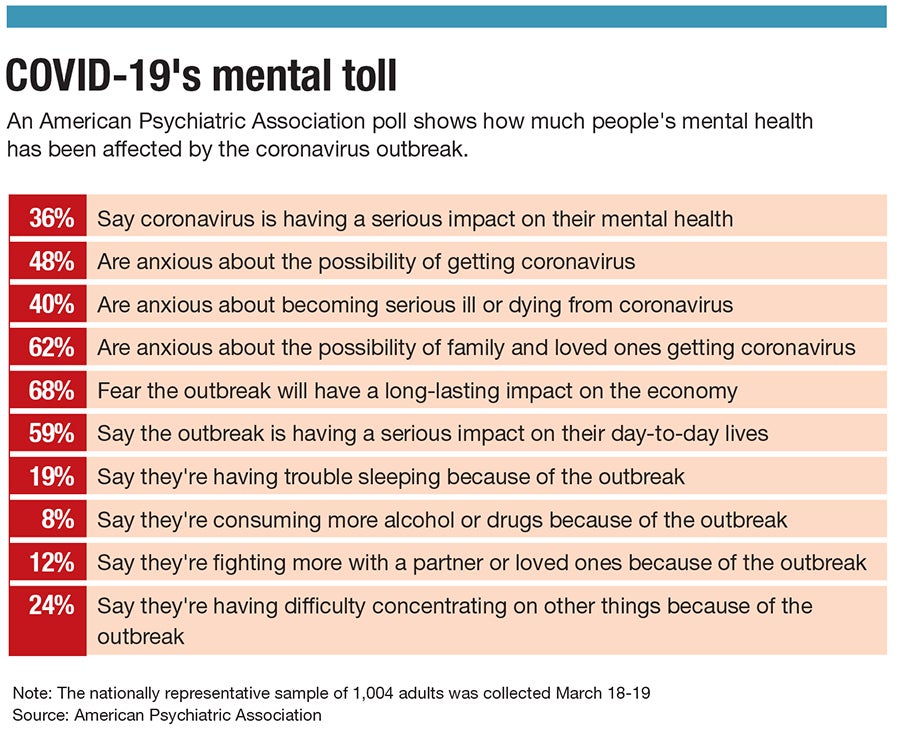
A March poll by the American Psychiatric Association backs that up.
More than one third of Americans said the outbreak was having a serious affect on their mental health, and almost one in five said it was causing them to lose sleep. In 8% of cases, the pandemic was causing them to drink or use drugs more.
“The stress and anxiety caused by the pandemic can and is having an effect on people’s physical and mental health,” Dr. Bruce Schwartz, the president of the association, said in a statement accompanying the poll results.
Making quick adjustments
For agencies in Central Massachusetts, the coronavirus pandemic hitting the state in a severe way starting in mid-March with government mandates for people to distance themselves from others meant clinicians had to quickly figure out how best to main services remotely.
Reliant Medical Group in Worcester converted its entire behavioral health department to be able to conduct video appointments with clients in 48 hours, including the time it took to train staff.
“That was a massive team lift,” said Sam Nordberg, Reliant’s chief of behavioral health.
At facilities with inpatient units, including AdCare and Spectrum, balancing social distancing requirements took more work.
AdCare’s 114-bed inpatient center in Worcester, for example, is still running largely as it would normally be except for adjustments to screen new patients more carefully. Daily group therapy sessions still take place, except in groups of three instead of two to give patients more space to spread out. A waiting room has only enough chairs so those waiting for appointments won’t have to be too close to one another.
“What we’re telling patients is, if you need to be here, we’ll take you,” said David Hillis, AdCare’s vice president of outpatient operations.

Spectrum, which has inpatient centers in Westborough and Weymouth, is taking patients’ temperatures during the admissions process and asking for risk factors as a way to determine if someone might have COVID-19. In Westborough, it has added a trailer outside its entrance to conduct screening away from others.
“We started screening right away, as soon as this came anywhere near Massachusetts,” said Lisa Blanchard, Spectrum’s vice president of clinical services.

Spectrum has changed how it allows patients to access medication. It’s typically required to be administered on-site in short doses, but some patients are being allowed to take home medication for up to 28 days to keep them from having to physically visit an office if they’re deemed stable enough.
Reliant, which has roughly 70 licensed therapists, conducted 700 or so video therapy sessions in the first two weeks once it went digital. Video is far preferable to phone calls, according to those in the field, because clinicians want to be able to see a patient’s facial expression or body language.
The agencies had to make sure they were complying with health insurance and industry regulations by going online. Reliant, for example, was able to have its Massachusetts-based therapists work with clients in Connecticut or New Hampshire because governors in those states waived requirements forcing therapists to be licensed in those states.
Next up has been moving group sessions online as well, something the agencies were tackling a few weeks behind first getting individual appointments running. The challenges include making sure all participants are able to have the computer technology or cellphone app allowing them to join. The hope is the online version can closely enough replicate the in-person benefits in camaraderie and support that clients offer one another.

The adjustment has been stark for places like AdCare, which Hillis said hadn’t done tele-health at all before now.
“It’s been very dramatic and very rapid,” Hillis said.
A critical time
These on-the-fly adjustments are coming at a time when continuing care is about as important as ever. The outbreak has left many anxious about what it means for their health or their loved ones’, or for their livelihoods.
“If you’re already highly sensitive to threats and worry about them, this new one will provide you new fuel for your anxiety and all your worry,” Nordberg said.
The first weeks of the pandemic’s hit locally was more about anxiety, Nordberg said. But that’ll likely shift more to depression as the weeks go on and people remain stuck largely in their homes and may suffer harmful feelings of loneliness.

Some manage their struggles by staying busy, Nordberg said, but that becomes harder if there isn’t a fitness club to work out, a cafe to meet a friend for coffee or a workplace to share with colleagues.
“What I've been telling people is we’ve come through the initial fear and stress event,” Nordberg said. “There’s no one who’s unaware now of coronavirus. At this point, we need to continue to manage stress of this new realization and the new world we’re living in, generally being much more isolated than before.
“Now we need to dig in for the marathon,” he added. “We’ve done the sprint.”
Hillis recommends people take time away from reading or watching the news and find simple pleasures, such as making a special lunch or dinner they can look forward to. Exercise or yoga can be critically important, he said.
Collins, who said she’s been in recovery therapy for years, said finding therapy online in the age of the coronavirus pandemic might not be ideal, but the services are there if needed.
“Tele-health, while it’s not perfect, it’s better than no connection at all,” she said. “Just keeping connected is the most critical factor. You need to see the faces and realize other people are doing this and I can do this.”

