Two years after policymakers enacted mental health care reforms designed to mitigate the problem, the share of patients experiencing long waits in Massachusetts emergency departments remains elevated, according to new state research.
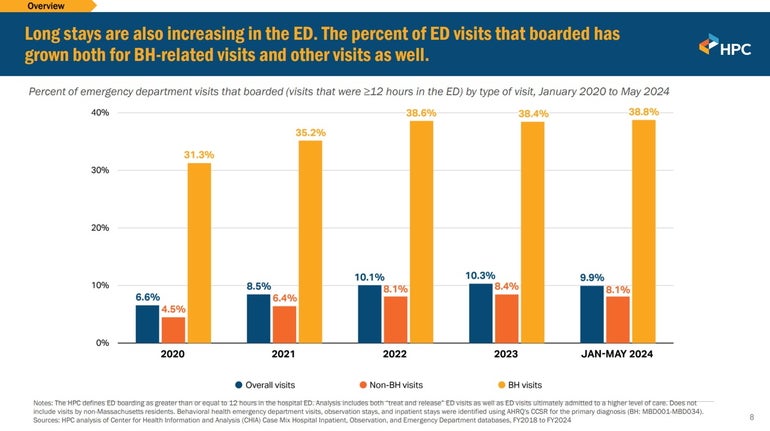
Nearly 39 percent of behavioral health-related emergency department visits lasted more than 12 hours before discharge or admission to a higher level of care between January 2024 and May 2024, up from 31.3 percent in all of 2020, researchers at the Health Policy Commission said Thursday.
Overall, the share of total trips that involved emergency department stays of 12 hours or longer has grown from 6.6 percent in 2020 to 9.9 percent in the first five months of 2024, researchers said.
The data presented at a commission meeting paint a harrowing picture of the boarding crisis, suggesting that Bay Staters in need still face long waits to access behavioral health care.
Boarding rates remained roughly the same from 2022 through May 2024 for both behavioral health visits and for other reasons that prompted patients to seek emergency department care, showing little change despite a 2022 state law that was intended in part to minimize emergency department boarding.
“This issue of hospital capacity is absolutely front of mind, not only to the HPC, but to many other state government agencies and the public,” said HPC Executive Director David Seltz. “Seemingly every other day, there is a story of long wait times to be able to get the care that is needed, long wait times in the emergency department.”
Researchers presented an analysis Thursday as part of a still-in-development HPC report, which when published later this year will also include recommendations to “alleviate what we’re seeing as clear bottlenecks within our health care system that are impairing the patient flow and impairing patient care,” Seltz said.
Behavioral health patients, including those with substance use disorder as well as other mental health care needs, could face long waits for a number of reasons including a lack of available, specialized inpatient beds and delays accessing psychiatric evaluations or lab tests.
The boarding crisis has been growing at the same time that hospitals struggle with capacity issues, driven in part by longer and more demanding patient stays.
In 2016, about 3.8% of hospital stays lasted longer than 30 days; by 2023, that had risen to 8.6%, according to data presented by HPC Director of Research and Analytics Laura Nasuti. While the number of hospital admissions decreased from 2018 to 2023, the average length of stay grew by an even larger rate, so total hospital use increased — leaving fewer open slots for people visiting emergency departments.
Providers and reform advocates have warned that lengthy emergency department boarding delays essential care for patients and burdens health care staff.
“Behavioral health boarding is harmful to the patients and their families, and it also impacts hospital staff, non-behavioral health patients in the emergency department, and emergency medical services,” Nasuti said.
Academic researchers, industry groups and state agencies all have different definitions of what constitutes behavioral health boarding in emergency departments. For its research, the HPC counted ED boarding as a patient spending 12 hours or more in the emergency department before either being placed to a higher level of care or being treated and released.
While the rate of patients boarding has increased across different reasons for visits, those with behavioral health issues are more likely to experience long waits.
In May 2024, nearly one in five emergency department visits for substance use disorder lasted 12 hours or more, as did close to half of all other mental health-related visits, according to the HPC.
Researchers said close to half of patients who boarded during a behavioral health emergency visit in 2023 received health insurance through MassHealth. Thirty-five percent lived in the lowest-income communities, 33% were nonwhite, and 17% did not have permanent housing.
Data show different trends for children and adults who spend even longer in emergency departments.
In 2022, about 52% of adults ultimately admitted to an inpatient psychiatric bed at an acute care hospital spent more than 24 hours in the emergency department. That share dropped to 40% for the span from January 2024 to May 2024.
But for children who were similarly admitted to an inpatient psychiatric bed in an acute care hospital, the share who spent 24 hours or longer in an emergency department has steadily grown, from 29% in 2020 to 45% in 2022 and 48% in the first five months of 2024.
The boarding crisis was a driving factor in the push for wide-reaching mental health legislation in 2022.
That measure eliminated a prior authorization requirement for mental health acute treatment, and it created a new process to expedite review and stabilization of emergency department patients younger than 18 in need of mental health care.
The HPC noted that Massachusetts also launched a Behavioral Health Help Line and a network of community behavioral health centers in 2023, which are open 24 hours a day to provide an alternative to the emergency department for some patients experiencing behavioral health crises.
Officials said the full HPC report will include more information on behavioral health boarding in other states as well as policy recommendations to rein in the still-potent crisis.
Lawmakers are weighing mental health funding as part of the annual state budget debate. In her spending plan, Gov. Maura Healey proposed slashing the number of case managers at the Department of Mental Health from 340 to 170, which opponents argue will prevent thousands of Bay Staters from accessing services.
Karen Coughlin, a registered nurse and a member of the HPC Board, said during Thursday’s meeting that Healey’s proposed cuts “could affect ED boarding moving forward.” She also pointed out the state lost some behavioral health beds when the formerly Steward-owned Carney Hospital in Dorchester shut down, and could lose more if Healey revives a now-paused plan to close Pocasset Mental Health Center on Cape Cod.
“I think we just need to be cognizant of some of the concerns that we are hearing from emergency room staff, that calls are still going unanswered, and that there could be the potential [for consequences], given the closures and the layoff of case managers who oftentimes, in lieu of [primary care providers], are the first line for behavioral health patients to avoid hospitalizations or moving further into behavioral health crisis,” Coughlin said.
Alecia McGregor, an assistant professor of health policy and politics at Harvard’s T.H. Chan School of Public Health and a fellow HPC Board member, called the presentation “eye-opening and concerning.”
Industry leaders will devote focus to the topic of behavioral health in children at an April 1 summit hosted by the Massachusetts Health and Hospital Association and Boston Children’s Hospital.