Central Massachusetts vascular surgeons are pioneering new devices, procedures, and service models to prevent the future healthcare system from being overwhelmed.
Get Instant Access to This Article
Subscribe to Worcester Business Journal and get immediate access to all of our subscriber-only content and much more.
- Critical Central Massachusetts business news updated daily.
- Immediate access to all subscriber-only content on our website.
- Bi-weekly print or digital editions of our award-winning publication.
- Special bonus issues like the WBJ Book of Lists.
- Exclusive ticket prize draws for our in-person events.
Click here to purchase a paywall bypass link for this article.
A perfect storm is brewing in the world of medicine, as the wave of an aging population collides with a shortfall of future surgeons.
Yet, the vascular surgery specialty in Central Massachusetts is breaking this troubling trend with technological innovation.
Central Massachusetts vascular surgeons are pioneering new devices, procedures, and service models to prevent the future healthcare system from being overwhelmed, while researching solutions for high healthcare costs and limited patient accessibility to the predicted shortage of surgeons.

Vascular surgery focuses on all the blood vessels throughout the body. This field serves an older demographic with an average patient age of 65 years and older. These patients typically have pre-existing conditions such as diabetes and heart disease further compounding their vein or artery ailments.
As medical advancements improve, people are living longer. While increased longevity is a favorable outcome for any patient, the patient load is clogging an already overburdened healthcare system as new patients are added to older populations, who are still receiving treatment well into their 90s and 100s.
“It is impossible at this current rate and pace that we are going to be able to keep up,” said Dr. Hector Simosa, who performs surgeries for the Vascular Care Group, which has locations in Framingham, Worcester, Leominster, and Sturbridge.
Game changer
Typically, Boston hospitals receive the spotlight when it comes to medical recognition, but Dr. Andres Schanzer, chief of endovascular and vascular surgery at UMass Memorial Medical Center in Worcester, has drawn patients to the hospital’s Center for Complex Aortic Diseases, one of 12 such centers in the U.S. and the only one in New England.
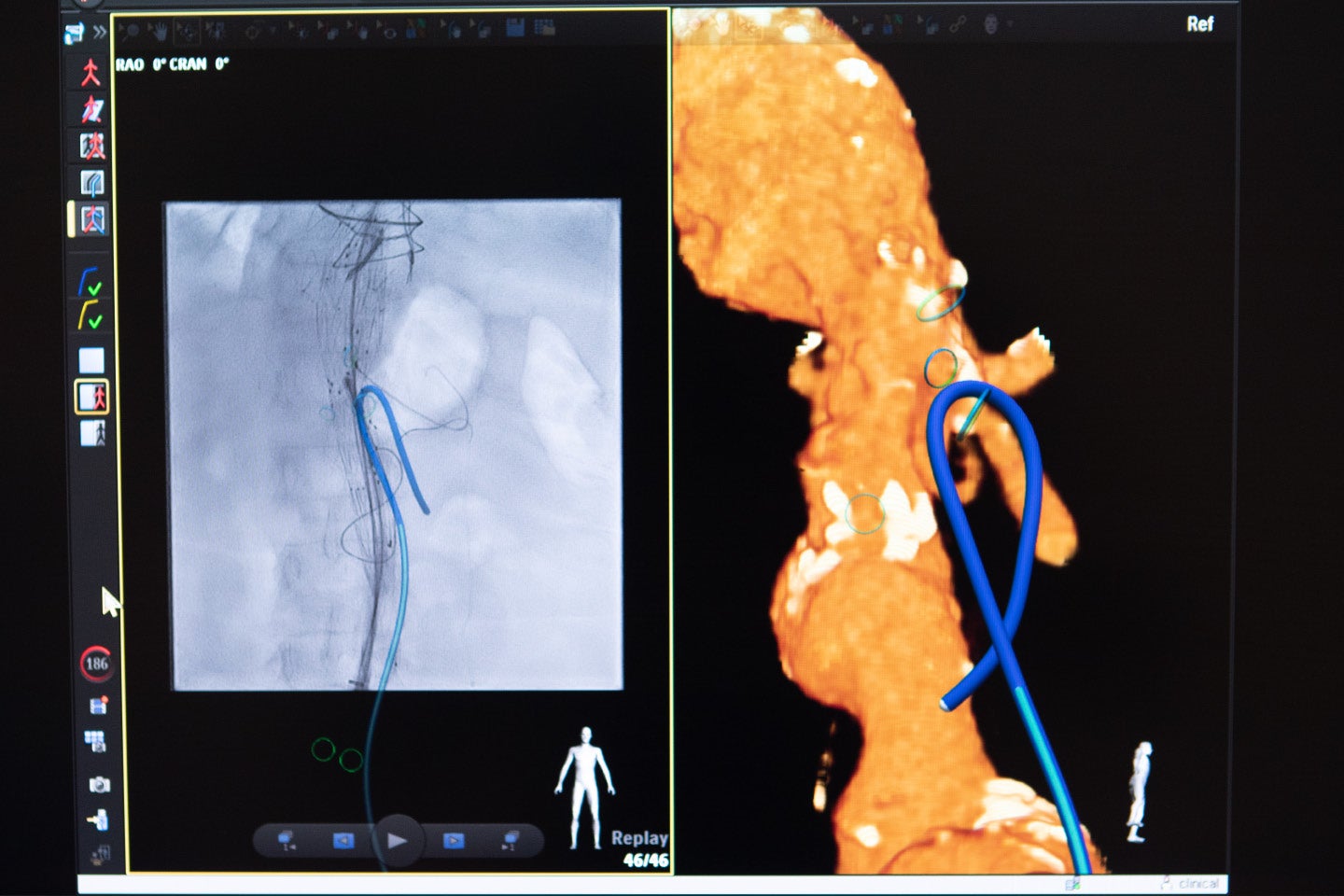
At UMass, Schanzer is using a minimally invasive procedure called the fenestrated endovascular aortic repair, allowing surgeons to repair the aorta through small incisions in the groin or arms while still preserving blood flow to the critical branch arteries in the kidneys and other vital organs of the body.
Prior to FEVAR, aortic repair was a large, open surgery requiring the chest and abdomen to be opened, and sometimes required the heart to be completely stopped in order to replace the aorta. This procedure came with high risks and long recovery times. Frequently, patients who were already ill couldn’t withstand it.
Now, FEVAR allows patients to receive stents in their blood vessels with minimal risk and significantly faster recovery times.
The UMass Center for Complex Aortic Diseases is only one of 10 sites fitted with the technology to prevent aortic aneurysms using minimally invasive surgery and stents.
These 10 sites are part of a clinical trial approved by the U.S. Food & Drug Administration, researching and evaluating the procedure. Schanzer has completed approximately 400 FEVAR procedures.
Schanzer said one of the most exciting advancements in vascular surgery is the use of Fiber Optic RealShape technology.
UMass became the first hospital in the U.S. to use this fiber optic light imaging to guide the aortic repair surgeries rather than relying on radiation, eliminating the large doses of X-ray radiation traditionally needed for the surgery.
“I would say that during my career, fenestrated and branched endografts, which are these advanced grafts we can use to treat these complex aneurysms, and Fiber Optic RealShape technology are the two most significant technological innovations I have seen across the entire field of surgery,” Schanzer said.

A rising need
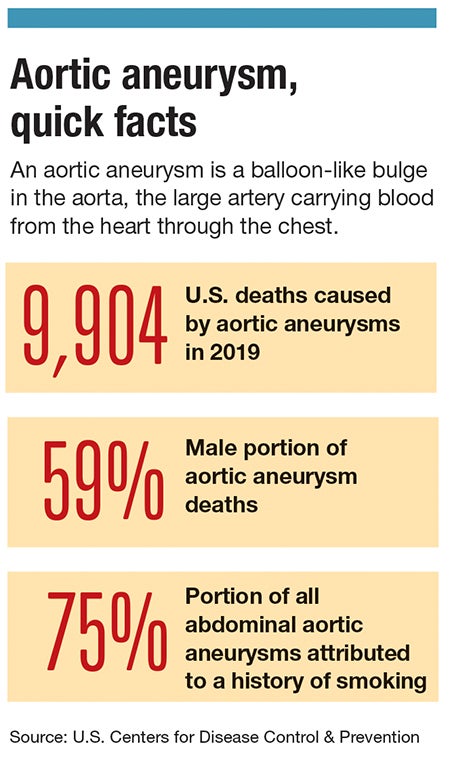
Aortic aneurysms account for about 10,000 U.S. deaths a year, according to the U.S. Centers for Disease Control & Prevention.
“Dr. Schanzer’s vision when he became division chief was one of really trying to build our volume and make us one of the highest-volume, academic vascular departments in the country; and along those lines he is pioneering these innovative techniques to manage complex aneurysm disease with a minimally invasive strategy,” said Dr. Jessica Simons, associate professor of surgery at UMass Medical School and program director of vascular surgery residency at UMass Memorial Health in Worcester.
The goal is to make the Center for Complex Aortic Diseases a sought-after destination for this type of care, even rivaling Boston hospitals.
“It is world-class care on par with any other institution, and for a lot of patients, it is just a bit closer to home and easier to get access to our system and then to navigate it once they are in the system,” said Simons, who became UMass Memorial’s first female vascular surgeon when she was hired in 2013. The vascular division is now majority women.
Having more innovative technology for vascular surgery will be important since the industry is expected to have a shortage of surgeons as the population ages and more vascular diseases arise, Simons said.
“Basically the prevalence of peripheral artery disease specifically is projected to just explode to be well over 200 million people worldwide, and so the need of vascular surgeons to care for that population is huge; and the current workforce is projected not to be adequate so if anything we need more vascular surgeons,” Simons said.
Simosa said reducing risk factors such as smoking, obesity, high cholesterol, and diabetes is key to making the disease more manageable for future doctors.
“Unless we do better in all of these areas, I do not think we are going to be able to put a dent in the pace at which the disease grows. This would eventually allow the doctors who are in training to be able to keep up and provide care for those folks,” Simosa said.
Reducing hospital costs
The Vascular Care Group, a group of interventional and vein centers throughout Massachusetts with locations in areas such as Worcester and Sturbridge, is implementing a business model elevating the patient experience while reducing costs and making healthcare traffic in hospitals more manageable.
This firm is revamping the patient experience by offering the latest in vascular technology with the convenience of receiving minimally invasive treatments in an office setting rather than a hospital.
While the Vascular Care Group did not invent this model, the surgery group is one of the few implementing this business strategy in the Northeast, said Simosa.
“We are emptying the buckets of our healthcare dollars. As healthcare costs continue to go up and up and up, we are using up all our Medicare and Medicaid funds, and the costs of private insurances keep going up,” he said.
Traditionally patients are sent to the hospital for appointments, preparations, procedures, and recovery, but many of these aspects can be completed in an outpatient, office-based setting, thereby reducing costs and decreasing the flow of patients to hospitals, which can focus on delivering care to severely ill patients.
“Just think of this, you have the same patient, the same doctor, the same procedure done in two different sites, same outcome; and you are saving at least 25% to 40% of the costs. If we do that across Medicare, we can extend the money for many many years to come,” Simosa said.
In addition to facilitating vascular procedures in a low-stress, outpatient environment, the Vascular Care Group is researching its own technological advancements in the vascular surgery field.
“This is not just an office full of doctors and administrators. These are people who are trying to think and come up with a solution,” Simosa said.

