A trio of researchers at UMass Medical School in Worcester are attacking the coronavirus pandemic from three different angles, as part of a $17-million Massachusetts effort to help the world combat the disease which has killed more than 400,000 people globally.
Get Instant Access to This Article
Subscribe to Worcester Business Journal and get immediate access to all of our subscriber-only content and much more.
- Critical Central Massachusetts business news updated daily.
- Immediate access to all subscriber-only content on our website.
- Bi-weekly print or digital editions of our award-winning publication.
- Special bonus issues like the WBJ Book of Lists.
- Exclusive ticket prize draws for our in-person events.
Click here to purchase a paywall bypass link for this article.
A trio of researchers at UMass Medical School in Worcester are attacking the coronavirus pandemic from three different angles, as part of a $17-million Massachusetts effort to help the world combat the disease which has killed more than 400,000 people globally.
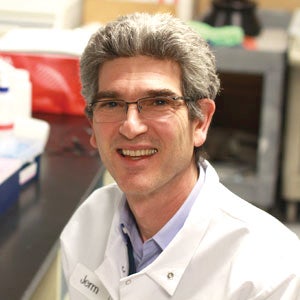
The researchers – Dr. Robert Finberg, Dr. Ann Moormann, and Dr. Jeffrey Luban – are studying ways to treat COVID-19, understand how it spreads, how people can be immune from its effects, and how herd immunity can be achieved.
“We would like to know a little bit more about exactly how the virus causes the damage that it does,” Finberg said.
The three UMass Medical School researchers are part of the Massachusetts Consortium on Pathogen Readiness, known as MassCPR, which is a statewide initiative including scientists and clinicians from Harvard University, the Massachusetts Institute of Technology, Boston University, Tufts University, University of Massachusetts, and local biomedical research institutes.
MassCPR is working to develop the infrastructure to address the COVID-19 pandemic. It was created through a research agreement between Harvard and the Evergrande Group in China, which is sharing financial support equally between Massachusetts research and researchers at the Guangzhou Institute of Respiratory Health in China. The funding is for five years.
MassCPR has obtained roughly $16.5 million to support and fund this first round of initiatives and projects. After receiving more than 400 applications for funding in March, MassCPR chose more than 60 applicants to receive funding, including the three at UMass.
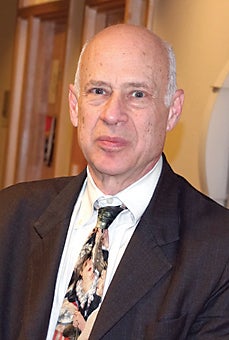
“This was obviously a very stiff competition, so anyone who actually received funding had an amazing application,” said Professor David Golan from Harvard Medical School, one of the faculty co-leads of MassCPR.
According to UMass Medical School, projects selected were for their potential to influence clinical outcomes within the next 12 months. Luban, for example, a professor of molecular medicine at UMass Medical School, is researching the virologic mechanisms of COVID-19, attempting to discover what makes it unique. He aims to precisely understand infectiousness of coronavirus with his research.
Host cells and antiviral possibilities
Finberg, chair of the UMass Department of Medicine, is researching how to identify and target host cells and genes crucial in addressing the COVID-19 pandemic. His background in studying respiratory viruses makes researching COVID-19 a natural shift.
“The questions I was interested in are one, whether we can find a drug to treat the virus … and the other was to find out exactly what cells the virus infects and what kind of cells respond to the virus,” Finberg said in a phone interview.
His project funded by MassCPR focuses on specifically these two parts, how disease is caused and if there could be a viral treatment. Finberg does this through studying human samples.
“Infectious disease can be defined in what cells the virus infects and what the host response is … both cause disease,” said Finberg.
Other than looking at the possibility of an antiviral agent to treat COVID-19 and how exactly the disease is caused, he is trying to understand how the virus works inside the body.
“Part of Dr. Finberg’s research has to do with finding so-called host targets that could be potentially drug targets that could help to prevent the infection of cells by the coronavirus,” said Golan.
Functional antibodies
Moormann, a professor at UMass Medical School who focuses on infectious diseases and immunology, is looking into one of the most popular current research topics in relation to COVID-19, functional antibodies, which help the body fight off the disease.

Her study measures the spectrum of functional antibodies, how long these antibodies last for, and how they differ in people of different ages. Antibodies indicate past infections.
“Part of the research I have funded is to look at the question of how long do the immunities to the virus that causes COVID-19 last,” said Moormann.
Though looking at human samples to see how many antibodies currently exist in a person is part of this project, her research has a more longitudinal element where she looks at how the antibodies change over months, getting samples three, six, and nine months after the initial sample.
“You can have an immune response that only protects you for a certain period of time, and it might be because your immune response doesn’t become a memory response but it helps clear the infection … We don’t know how long [COVID-19 antibodies] last,” said Moormann.
Moormann gets samples from patients who have recovered from coronavirus but also from people who were not diagnosed. She recruits study participants that are healthy and that are patients. She then tests to see whether or not the individual has antibodies.
Participants can choose to give a sample once, or, for those who want to be in the longitudinal part of the study, choose to come back in the following months to give more samples.
“I want to look beyond [a few months]. Like in six months, in nine months, do you still have antibodies? Are you still protected?” Moorman said.
Her research is a necessary part of understanding if and how herd immunity can be achieved to stop the COVID-19 pandemic.
Moormann’s research is one of the very hottest topics right now in thinking about the pandemic, Golan said.
“It’s incredibly important for two reasons. One is when people get coronavirus infections, they develop the antibodies and it’s a question whether those antibodies protect you against another infection of coronavirus,” said Golan.
A communal effort
Each of these doctors’ research projects aims to understand COVID-19 better so they are able to correctly fight against it which is why they obtained crucial funding from MassCPR.
MassCPR has been able to create a community of researchers and scientists in Massachusetts that have come together to better understand and control coronavirus. Golan said the collaboration and sharing of data between researchers is a key part of MassCPR and is already leading to important findings.
“One thing that has been hugely highlighted by this pandemic is that we weren’t too well prepared for it,” Golan said. “It’s our obligation to the next generation to be ready for the next one in a better way.”

