About 82,000 Bay Staters lost MassHealth coverage in August, another sizable drop in enrollment as the state reaches an “inflection point” in a year-long effort to review eligibility for every single member.
Total enrollment in MassHealth, which combines Medicaid and the Children’s Health Insurance Program under one umbrella, fell for the third straight month with additional drops forecast in the near future, officials announced Thursday.
Massachusetts is now five months into a campaign to determine how many of the 2.4 million people on MassHealth rolls in April still qualify for the publicly funded health insurance. The federal government prohibited people from losing Medicaid coverage during the pandemic. That policy has since ended, requiring all 50 states to embark on a similarly gargantuan review.
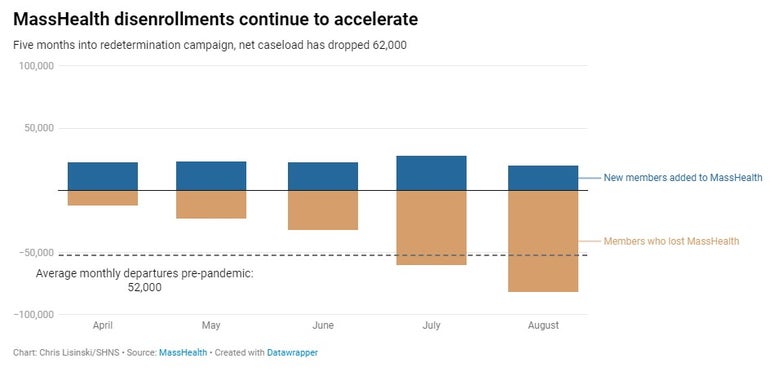
So far, a total of about 208,000 people have departed MassHealth since April 1, according to the latest state data. Normal new enrollments have continued in that span, cutting the net drop in the caseload to about 64,000 or 2.66 percent.
In August, about 20,000 new enrollments — which officials described as “within a typical monthly range” — offset the 82,000 disenrollments, leading to a net caseload drop of 62,000 people. Before COVID-19 hit, the state typically removed about 52,000 people from MassHealth per month.
Assistant Secretary for MassHealth Mike Levine said officials are so far “seeing what we expected.”
The administration projected before the campaign began that it would lead to a net reduction of 300,000 to 400,000 people over the course of the year, freeing up $1.9 billion in state funding in fiscal year 2024 to be spent elsewhere.
Levine said Thursday the next two months should give a much better sense if that forecast remains accurate.
“I would say we’re at an inflection point right now. We’re starting to see, again, the more significant drops, and we’re going to see that through the fall. So I’ll have a much better answer for you in I’d say two months based on two more months of experience,” Levine said. “But nothing that we have seen yet suggests we’re in a very different ballpark than that [300,000 to 400,000].”
While MassHealth numbers continue to drop, the Massachusetts Health Connector marketplace has been adding more and more people, especially to subsidized and ConnectorCare plans.
Officials estimated that about one-quarter of people who lost MassHealth coverage newly enrolled in what Levine described as “affordable, subsidized coverage on the Connector.”
About 49 percent of Bay Staters who have lost MassHealth coverage since April were found no longer eligible following the redetermination review, and 48 percent were removed from the rolls because state officials did not have enough information to conclude whether they still qualify. Another roughly 3 percent, or about 6,100 people, were removed from MassHealth because the state was unable to contact them.
The roughly even split differs from the trend across the rest of the country. Among all states with available data, nearly three-quarters of people who lost Medicaid had their coverage terminated for “procedural reasons” such as incomplete paperwork, according to data tracked by nonprofit health policy organization KFF.
However, the share of Bay Staters removed from MassHealth because they did not submit enough information or could not be reached has increased compared to earlier months.
“We’re starting to see this group climb similar to what we’ve seen in other states who started this process prior to us,” said MassHealth chief operating officer Elizabeth LaMontagne.
Officials said Thursday that MassHealth inadvertently disenrolled 4,851 people because their household failed to respond to renewal paperwork, a process that did not comply with federal guidance calling for more granular review of each member on a person-by-person basis.
States can automatically renew Medicaid or CHIPS recipients based on already available information like wage data, and the federal Centers for Medicare and Medicaid Services wants that process to happen at the individual level rather than determining an entire family or household’s status at once. Eligibility requirements can differ based on age, so many children will remain eligible for Medicaid even if their parents no longer qualify.
CMS announced Thursday that 30 states including Massachusetts either are not conducting automatic renewals at the individual level or are still working to reinstate people affected by the issue.
Federal regulators raised specific concerns about children losing coverage, though MassHealth officials said they do not believe any children were impacted by the inadvertent disenrollment of 4,851 people. Unlike several other states, Massachusetts did not list children as a population affected by the household autorenewal issue in its response to CMS.
Officials here pointed out that even while the overall size of the rolls has dropped, MassHealth enrollment among people 20 and younger has increased from about 806,000 in April to 819,000 in August, data show.
“What some states are doing is saying, ‘Well, if anyone in the household needs to respond, and they don’t respond to a renewal, then we’re going to close the whole household,'” Levine said during a morning briefing with reporters. “That is happening in other states. That is not happening in Massachusetts.”
“So if you’ve got two parents and two kids and we are able to autorenew the kids based on their income, we autorenew the kids based on their income,” he added. “If the parents don’t respond to a renewal form, those parents will lose coverage, but the kids stay covered.”
CMS said it would require states to reinstate Medicaid coverage for about half a million children and families across the country.
MassHealth is in the process of reinstating those 4,851 affected people, an official said.
The agency has not published data through its dashboard summarizing how many people were found still eligible to remain covered following a redetermination review. About 3,600 people who joined the MassHealth rolls in August had been disenrolled less than three months earlier. Levine said those individuals were “very likely eligible” to retain coverage all along but lost it because of paperwork reasons.
“We need to keep a really close eye on that metric as we go through the fall,” he said.