Confronting the strained primary care workforce and state residents struggling to get basic preventive care, Massachusetts health regulators recommend reducing administrative burdens, growing the talent pipeline and expanding investments.
The Health Policy Commission released a report Thursday delving into a shortage of new providers entering the field, low reimbursement rates compared to specialty care, unsustainable workloads and burnout, and a high volume of patients turning to the emergency room because they couldn’t access a primary care clinician.
The HPC also outlined recommendations for lawmakers, health care organizations, and public and private insurers aimed at shoring up the primary care field. The recommendations will be honed and expanded through a new primary care task force created through the new hospital and market oversight law.
“The state of primary care in the United States and in Massachusetts is in a state of extreme challenge, and the need for action and policy action to improve both the delivery of care and to support the primary care workforce is urgent,” HPC Executive Director David Seltz told board members Thursday afternoon. “And so we at HPC will be working to really the support the work of this task force, dedicating our staff and resources and time to this task force. I expect that we will be moving with urgency on the mandates of this task force.”
Gov. Maura Healey and Senate President Karen Spilka have expressed interest recently in investing in primary care, although concrete plans have not emerged. State officials are crafting fiscal 2026 spending plans based on a 2.2% tax revenue growth estimate, and facing pressure to bring down soaring health care costs.
Seltz suggested his agency may need more financial and staffing resources this budget cycle to carry out the “ambitious” mandates from the new hospital oversight and prescription drug reform laws, which creates new offices at the HPC, including those focused on pharmaceutical policy and health care resources.
“We’ll be working with our partners in the Legislature in this budgetary process to work with them and to model out what we think the actual budgetary impact will be in this first year and in the years to come, as many of these will be multi-year efforts,” Seltz said.
Measured against 15 U.S. metros, Boston logged the second-longest wait times for a new patient appointment for a physical in 2022. Just over 40% of Bay Staters said they struggled to access care in 2023, and about two-thirds of residents in a survey said they turned to the emergency department since they couldn’t schedule an appointment soon enough at a doctor’s office or clinic.
Compared to other states, Massachusetts has “among the lowest shares of physicians working in primary care,” the HPC said.
The state had roughly 15,000 primary care providers in 2022, and the provider mix is changing. The percentage of providers who are nurse practitioners or physician assistants increased from 26% to 31% from 2018 to 2022, the HPC said.
Massachusetts’ aging primary care workforce is also exacerbated by a low rate of new providers joining the field. Only one in seven new physicians here went into primary care in 2021. The HPC said employment in Massachusetts physician office settings has “barely increased” since 2019 despite a more than 10% rise nationwide.
The share of Massachusetts primary care physicians in direct patient care, measured across total physicians, dropped from 26.7% to 24.7% from 2014 to 2020. Meanwhile, the share of specialty physicians grew from 69% to 70.7%.
To bolster the primary care workforce, the HPC recommends Massachusetts should resume and expand the scope of Medicaid funding for graduate medical education, including residencies. Health officials say Massachusetts discontinued that Medicaid model in 2010 and is one of seven states whose Medicaid programs don’t cover costs for clinical training.
The state should also invest in loan repayment programs for nurse practitioners and physician assistants, and adjust supervisory requirements for PAs to provide care, the HPC recommends.
Health regulators attribute some of the sector’s challenges to lower payment rates for primary care compared to specialty services and hospital-based care. Medical school graduates with hefty student debt gravitate toward specialty care where they can earn significantly more than in primary care, the HPC said.
“Common specialty procedures may be able to generate more revenue in one or two hours than a primary care physician would receive for an entire day of caring for patients,” Sasha Albert, the HPC’s associate director of research and costs trends, said.
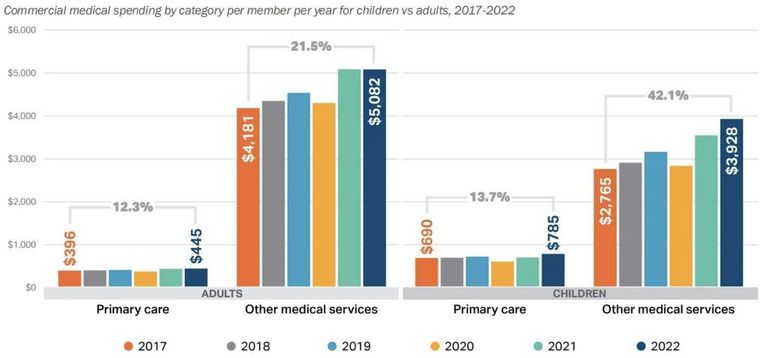
From 2017 to 2022, the HPC found primary spending in Massachusetts grew only half as fast as spending on all other medical services. As a percentage of all commercial spending, primary care spending dropped from 8.4% to 7.5% during that time period.
“This dynamic is particularly striking for children,” HPC senior research associate Charlotte Burlingame said. “Primary care spending just grew one-third as fast for children compared to spending on all other medical services.”
Massachusetts should increase spending for primary care by shifting payment models and rebalancing overall medical spending, the HPC said. Insurers should embrace capitated payment models for primary care — in which providers receive predictable and upfront payments to cover patients — and support independent primary care practices and community health centers, health officials recommend.
HPC Commissioner David Cutler mentioned the state’s past efforts that pushed insurers to pursue alternative payment models to increase demand for primary care. He said that prompted some big health systems to invest in primary care but suggested that “maybe hasn’t gone far enough.”
“Massachusetts has more alternative payment model use than anywhere in the country, at least we used to as of a couple years ago. We tracked it,” Cutler said. “So how is that not having some kind of effect on the demand for pay, for work conditions of primary care docs?”
Albert said primary care’s fee-for-service model is a “big part of the picture.”
“If the only activity of primary care that’s paid for is when the clinician is in the room with the patient, there’s a lot of work of primary care that doesn’t cover,” Albert said. “That doesn’t cover the hours of patient correspondence through myChart and other patient portals. That doesn’t cover negotiating with insurance companies.”
Administrative burdens in primary care can cause providers to leave the field or reduce their patient load as they experience burnout. Referencing other studies, the HPC said primary care physicians “spend anywhere from equal to double the amount of time on administrative work as spent in direct patient care.”
To alleviate administrative burdens, the HPC recommends that insurers overhaul program requirements, including those tied to billing, coding and prior authorizations. Health care organizations should also increase wages for care team staff to reduce turnover and better support patients and clinicians, the HPC said.
Albert said the HPC hopes its report can help the task force as it examines strategies to improve care access, delivery and financial sustainability. Members must propose payment models to increase reimbursement for primary care services and establish a primary care spending target for public and private insurers.
Massachusetts could also incorporate lessons from other states, health officials say. Rhode Island requires that insurers allocate at least 10.7% of their medical spending on primary care. California wants primary care to account for 15% of total health care spending by 2034, while Washington has set a target of 12%.
HPC Vice Chair Martin Cohen requested the task force also explore the intersection between primary care and behavioral health.
“It’s primary care where early screening is happening for both mental health and substance use cases, and it’s also where a great deal of treatment is taking place through prescriptions or also with referrals to behavioral health practitioners,” Cohen said. “In the behavioral health side, we’ve been pushing for integrated care models (for) primary care and behavioral health to lower the cost of health care for patients.”